A team at the University of Alberta has developed an exciting new combination of existing technologies which will simplify and speed up prostate cancer detection and determination of its nature, and be as accurate as physical biopsies.
John Lewis is an associate professor in experimental oncology, in the Department of Oncology at the University of Alberta, and the Frank and Carla Sojonky Chair in Prostate Cancer Research.
Listen
Professor Lewis is co-author of a study published in the journal Cancer Research, which is entitled Enhanced detection of cancer biomarkers in blood-borne extracellular vesicles using nanodroplets and focused ultrasound. (abstract and full PDF HERE)
Typically men will get a simple blood test for the presence of PSA (prostate-specific antigen), if the level is high it might indicate the presence of a prostate cancer. To be sure however, a biopsy is required. This is a highly invasive and unpleasant experience.
Lewis says that men with low grade prostate cancer can decide to monitor the disease, but that usually involves getting this invasive biopsy every year or so. Because of this he says, “Many people opt for surgery instead of more biopsies. It is clearly something we need to improve upon.”
New technique would be faster, simpler, and non-invasive
That improvement seems well on the way. This new procedure uses two known technologies and combine them for the first time in a rapid non-invasive procedure which is also as accurate as biopsies.
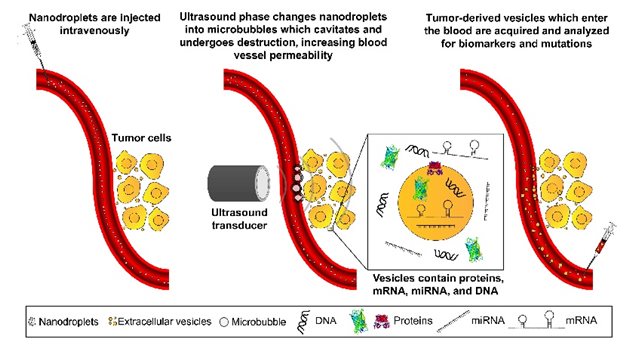
A simple injection of nanodroplets into the blood starts the procedure, focused ultrasound is then applied to the prostate tumour, and a blood sample then drawn off.
Neither nanodroplets/microbubble or ultrasound have any effect on their own, but when ultrasound is applied to the nanoparticles at the tumour they absorb the energy and expand into microbubbles. These then bump and press against tumour cells knocking off vesicles into the blood stream. When a subsequent blood sample is taken the now numerous specific tumour vesicles in the blood (with their genetic material) can be analysed in the lab to determine the nature of the tumour far more comprehensively than the biopsy. It can also provide personalized information about the tumour and any specific mutations and the optimum treatment chosen for that type of tumour.
Further work is proceeding on increasing the amount of key vesicles released into the bloodstream through the technique, focusing on the biomarkers that are of the most importance.
Because the technologies are widely accessible and are already being used in other procedures, Lewis and the team feel the lab trials will soon be performed in clinical trials, and from there become available to medical professionals.
Funding for this research came entirely from philanthropic sources via the Alberta Cancer Foundation and Prostate Cancer Canada.






For reasons beyond our control, and for an undetermined period of time, our comment section is now closed. However, our social networks remain open to your contributions.